Employer-provided health coverage is a major perk— if not a must-have— for jobseekers in the United States. According to a study from the Society for Human Resource Management, 46% of employees with employer-sponsored plans said health insurance was either the deciding factor or a positive influence in choosing their current job. Furthermore, 56% said that whether or not they like their health coverage is a key factor in deciding to stay at their current job.
Even if you know you want to take advantage of your company’s healthcare offerings, you may feel a little lost at sea when it comes down to choosing the right insurance plan for yourself and your family. In this article, we’ll break down some of the basic things to consider to help you evaluate your options.
How to choose a health insurance plan from your employers
Here are four simple steps to help you choose the best insurance option.
1. Understand the types of health insurance plans
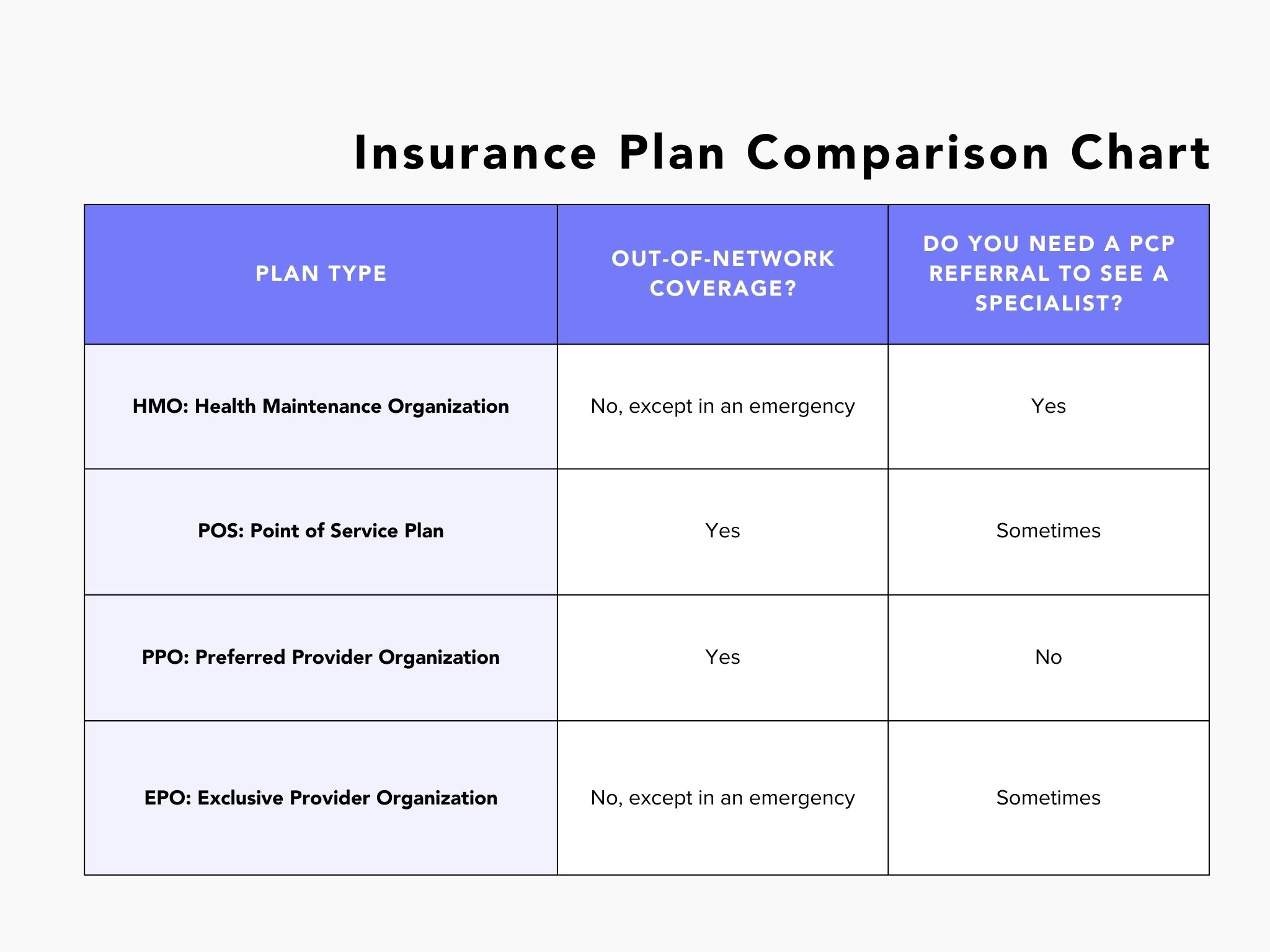
There are four main types of health insurance plans: HMO, POS, PPO, and EPO. One of the main differences between plan types is whether or not they offer any type of out-of-network coverage.
In short, a network is a group of healthcare providers— doctors, hospitals, labs, and more— that are contracted with an insurance company to offer services to members of that health insurance plan. These facilities and doctors must meet certain credentialing requirements and agree to accept a discounted rate for covered services under the health plan in order to be part of the network.
In-network healthcare providers are those that are a part of the network and accept your plan.
Out-of-network providers have no contract with your health plan and can charge you a higher, full-price rate for their services.
Another big differentiator is whether or not a plan requires that you have a referral from your primary care physician (PCP) to see a specialist.
RELATED: What Employee Benefits to Look for When Job Hunting
2. Get familiar with health insurance terminology
You might encounter some jargon that you are unfamiliar with as you look over your plan.
Luckily, HealthCare.gov provides a great glossary of terms! Here are a few of the big ones that you’ll want to know.
Premium
This is the amount you pay for your health insurance every month. Your employer may cover a portion or all of your premium each month.
Keep in mind that a lower premium doesn’t necessarily mean more savings. Depending on your healthcare needs, paying a little more each month may translate to a better plan and more savings at the doctor’s office.
Deductible
Your deductible is the amount you pay for covered health care services before your insurance plan starts to pay. For example, with a $3,000 deductible, you pay the first $3,000 of covered services.
After you pay your deductible, you usually pay only a copay or coinsurance for covered services and your insurance company pays the rest.
Out-of-pocket maximum
Your out-of-pocket max or out-of-pocket limit is the most you have to pay for covered services in a plan year. After you spend this amount on copays, deductibles, and coinsurance for in-network care and services, your health plan pays 100% of the costs of covered benefits.
Copayment or copay
A copay is a flat fee that you pay each time you go to your doctor or fill a prescription. The remaining balance of your visit is covered by insurance.
Copays can happen one of two ways: immediately or after you’ve met your deductible. If your copays apply only after your deductible has been met, you will pay the full out-of-pocket cost for your doctor’s visit until you hit that number. If they apply immediately, you will only pay the flat fee whenever you visit, regardless if you’ve met your deductible yet.
Coinsurance
Coinsurance is the percentage of costs of a covered health care service you pay after you’ve paid your deductible. You will pay this percentage until you reach your out-of-pocket maximum.
For example, a common coinsurance amount is 20%. This means that after you reach your deductible, you will pay 20% of your healthcare expenses and insurance will pick up the other 80%.
3. Evaluate your and your family’s needs
Now that you better understand how different plans work, start thinking about how you expect to use your plan. This is perhaps the most important part of this process, as the best plan for one person may be the worst option for another based on individual or family needs.
Some things that you want to think about for yourself, spouse, and dependents include:
- How often do you visit your primary care physician?
- How often do you visit healthcare specialists?
- Do you have an upcoming surgery?
- Do you have a chronic condition, such as diabetes, heart disease, or cancer?
- What prescriptions do you take on a regular basis?
- Do you frequently seek emergency care?
- Do you get lab work done regularly?
- Are you expecting a baby or plan to have a baby in the near future?
- Is mental health coverage important to you?
If you are generally pretty healthy and only find yourself only going to the doctor once a year for checkups, a low-premium, high-deductible plan may be the best option for you. On the other hand, if you fill several prescriptions each month and see your doctor frequently, you may want to opt for a plan that you pay more for each month but saves you more on the healthcare services you use the most.
4. Compare offered plans
After you evaluate what, exactly, you need from a plan, you can look at the options that your employer has provided you.
Comparing benefits
Each plan should have a summary of benefits that explain what it covers and what it doesn’t. Go through the benefit summaries for each of your options, taking note of which ones check the boxes of your healthcare needs.
Comparing networks
If you wish to continue seeing your current doctors and healthcare providers, you’ll want to look at whether or not they are in a plan’s network. You can see if a doctor is in-network by visiting the carrier’s website or calling your doctor’s office directly.
Comparing costs
Next, compare the out-of-pocket costs of each plan. Compare your monthly premium to your expected savings based on the coverage and your average healthcare needs.
Take your time and ask questions
While you’ll certainly want to make your selection before the enrollment period ends, take your time to choose the plan that will be most beneficial to you. If you have questions, don’t hesitate to ask a member of your employer’s HR or People team. You can also contact the insurance provider or representative from their enrollment team if you have questions about a specific plan and what it covers.
